Dysautonomia: What It Is and Why It's Important
Dysautonomia is a group of potentially devastating conditions that are oftentimes misunderstood, misdiagnosed, and treated improperly. Because of the confusion around them, you might think they’re uncommon; however, dysautonomia affects over 70 million people worldwide. It also affects people of all ages, races, and genders. When someone walks through our practice doors who is not sleeping well, has fatigue, and has pain that jumps around to different places in their body, we always look into dysautonomia.
Dysautonomia refers to a group of neurological disorders in which the autonomic nervous system (ANS) has gone awry. Though there’s no “cure” at the moment, getting to the root cause can improve these conditions significantly.
If you remember from biology class, the ANS is the part of the nervous system that works without a person’s conscious effort. Its responsibilities include things like controlling blood pressure, heart and breathing rates, body temperature, digestion, metabolism, urination/defecation, body fluid production, and sexual response (1). These are all things that your body does without you thinking about it.
You may control some of the actions that lead to the ANS response, but you do not control your ANS response. For example, when you decide to run, your ANS responds by faster breathing and sweating. When you engage in an unhealthy disagreement, your ANS may respond by increasing stress responses. When you decide to pray or meditate, your ANS may respond by lowering stress responses.
The ANS includes both the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is the part of the nervous system that is “fight or flight,” meaning that it responds to a perceived threat or stressor. The parasympathetic nervous system helps to bring the body back to a calm state.
Dysautonomia can affect the sympathetic nervous system, the parasympathetic nervous system, or both, and its effects can be mild or they can be severe and debilitating. Symptoms can also wax and wane or be unremitting.
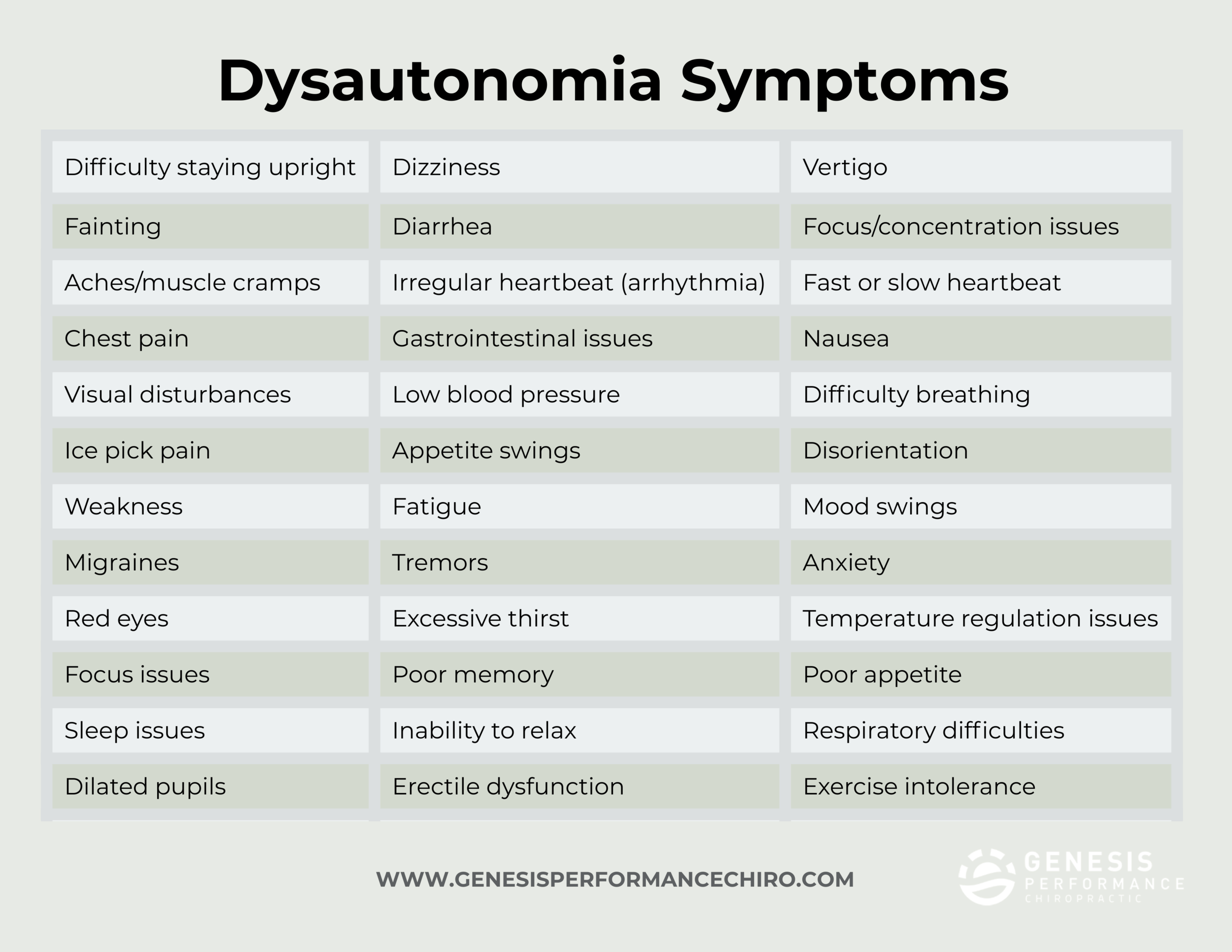
While symptoms are extremely varied (see the image below), those who are affected are often given different diagnoses that don’t explain the totality of their conditions. Examples of misdiagnoses include chronic fatigue syndrome (often a “catch all” diagnosis), panic attacks, irritable bowel syndrome, and fibromyalgia. Or they’re unfortunately written off as being mentally unstable. We often see cases in which the patient has not been taken seriously by other medical practitioners, when in fact, their symptoms are quite real and serious.
Types of Dysautonomia
There are various types of dysautonomia. We name and describe a few below (3).
Neurocardiogenic syncope (NCS): NCS is the most common type of dysautonomia. It consists of fainting spells, which may occur only a couple of times in a person’s lifetime or multiple times a day.
Postural orthostatic tachycardia syndrome (POTS): POTS is a disorder that involves blood circulation issues. In POTS, when an affected person moves from a horizontal to an upright position, they have a tremendous increase in heart rate, or a tachycardia. They may experience fainting, chest pain, lightheadedness, and shortness of breath. They may also experience symptoms such as GI distress, exercise intolerance, shaking, and temperature sensitivity. POTS is five times more likely in females than males.
Familial dysautonomia (FD): This is an inherited type of dysautonomia, which can include a decreased sensitivity to pain and hot/cold temperatures, lack of tear production, and issues with body temperature and blood pressure regulation. It is more common among Jewish people from Eastern Europe.
Multiple system atrophy (MSA): MSA is a progressive neurological disorder that can become life-threatening. MSA affects three main parts of the brain: the basal ganglia, the cerebellum, and the brain stem. MSA’s effects on the brain can result in issues with balance, movement, and unconscious body functions (i.e., bladder control). MSA is often mistaken for Parkinson’s disease, though MSA has more widespread autonomic nerve damage.
Physicians often classify MSA as either Parkinsonian-like (MSA-P) or with a type that has more cerebellar dysfunction (MSA-C). MSA-P patients often have more tremors, muscle rigidity, and slowness of voluntary movements. MSA-C patients have more lack of control over gait and limbs.
Early symptoms of MSA may include lightheadedness, dizziness, fainting, dilated pupils, and/or headaches, while later stage symptoms of MSA may include heart arrhythmias, difficulty chewing or swallowing food, or difficulty speaking. In any stage of MSA, one may have difficulty making facial expressions, muscle rigidity, loss of fine motor skills, loss of bowel control, as well as a plethora of other life-changing symptoms.
MSA is often seen in patients who are over 50, with men being more likely to develop the condition than women. However, women and those younger than 50 can still develop MSA (4).
Pure autonomic failure: Symptoms of pure autonomic failure include dizziness, fainting, vision issues, fatigue, and chest pain. The main symptom of pure autonomic failure is orthostatic hypertension, which is an extreme and sudden drop in blood pressure when standing. People with pure autonomic failure also have abnormal blood pressure responses to everyday activities.
As noted before, dysautonomia in general is much more common than you might think, affecting more than 70 million people worldwide. It may be present at birth, it may develop over time, or it could appear suddenly.
Dysautonomia Symptoms
There are quite a variety of symptoms with a diagnosis of dysautonomia. See our chart below for symptoms that are associated with dysautonomia (5).
Because of the variety of symptoms and issues that dysautonomia can cause, it is often not addressed properly. We see this often in functional medicine cases. For example, if a person with probable dysautonomia goes to see a cardiologist, the cardiologist may focus on arrhythmias and not see the connection with the other symptoms. If the person goes to see a gastroenterologist, the gastroenterologist will look for digestive issues, but perhaps lose the big picture. It’s important to have a whole person and multi-system approach when addressing someone with dysautonomia.
Dysautonomia Causes
Dysautonomia may also have a variety of causes (6), sometimes due to other conditions, making it more complicated to diagnose.
With the various types and causes of dysautonomia, it’s important to have a practitioner that takes a full medical history and does a variety of labs to determine root causes. We can help you to understand the pieces of the puzzle. Please contact our office if you suspect that you or a loved one has dysautonomia. And look out for our next article, which dives more into some of the causes of dysautonomia.
Works cited:
Vinik, A. I. (2012). The conductor of the autonomic orchestra. Frontiers in Endocrinology. https://doi.org/10.3389/fendo.2012.00071.
https://my.clevelandclinic.org/health/diseases/6004-dysautonomia