A Functional Medicine-Based Approach to Hormone Replacement Therapy
The hormonal changes that occur during menopause bring about some significant changes for most women. As the reproductive cycle comes to a close, the production of many important hormones decreases greatly, which can cause a myriad of problems. Women may experience a variety of unpleasant symptoms, from hot flashes and weight gain all the way to increased UTIs and even cognitive decline. Many of these problems can be traced back to the changes in hormone production. Most women just never feel the same and struggle to feel like themselves again.
Symptoms include:
Increased UTIs
Vaginal dryness, itchiness, and pain
Increased yeast infections
Headaches
Mood changes
Memory loss
Depression
Anxiety
Hot flashes
Night sweats
Joint pain
Weight gain
Sleep disturbances
Why can’t women just take estrogen?
We’ve talked at length about estrogen in this series and the effects of the decreased levels of estrogen on women. So why don’t women just take estrogen hormones to alleviate these issues? While estrogen supplementation, in the form of estradiol, can be beneficial for alleviation of some symptoms, it is not the hormone women need when they go through menopause. Research has found that hormone therapy in the form of estrogen-progestin pill increases the risk of conditions such as heart disease, stroke, blood clots, and breast cancer (1). It also can increase inflammatory markers, such as C-reactive protein, in the body (2).
Looking beyond estrogen and testosterone
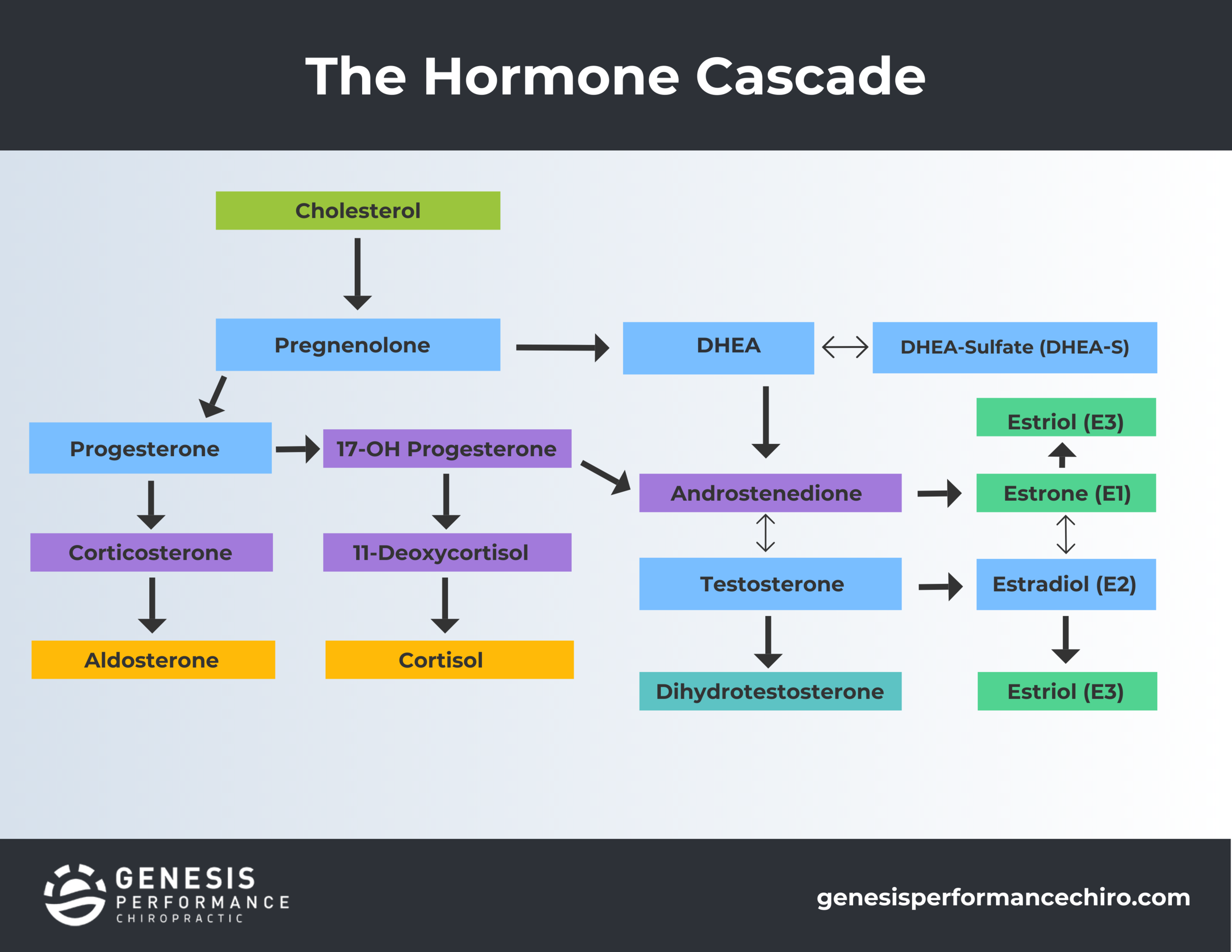
While estrogen and testosterone are important end products, there are more than just a couple of hormones that are affected by the changes that occur with menopause. In fact, there are SEVERAL hormones. Some of these hormones are called precursor hormones. Precursor means “a thing that comes before another.’ When we are talking about hormones, we mean precisely that - hormones that come before or are converted into other hormones. This supply of precursor hormones influences the supply or amount of other hormones.
Without precursors, we miss the benefits of the full hormonal cascade working together for the benefit of the body as a whole. Each precursor plays a role in our health and well being. If we miss the precursor, we can miss its benefits. This does not mean that there is not a benefit to taking hormones like estrogen or testosterone. There are times when taking estrogen or testosterone is needed because a patient cannot convert well even with all the right amounts of precursors. But, the amount of estrogen or testosterone will be less because the entire hormonal cascade is being fed. If you go straight to hormones like estrogen and testosterone and do not include a well rounded hormonal program, you will lose the many benefits of the other hormones. Each hormone, whether considered a precursor or not, has specific benefits to the body. We will review many of these precursor hormones and their benefits below.
Pituitary and adrenal gland hormones
Our bodies rely on endocrine glands to make hormones. The primary endocrine glands are the pituitary, pineal, thymus, thyroid, and adrenal glands as well as the pancreas. Many of the precursor hormones come from the pituitary or adrenal glands. Adrenal glands are located above the kidneys, and they produce important hormones, such as sex hormones and cortisol. They produce these hormones in response to signals from the pituitary gland, which is located in the brain. The pituitary gland, also located in the brain, responds to signaling from the hypothalamus, also located in the brain. While this is not an exhaustive list, we want to share some important hormones produced by the pituitary and adrenal glands.
Two hormones produced by the pituitary gland (specifically, the anterior pituitary) are:
Follicle-stimulating hormone (FSH)
Luteinizing Hormone (LH)
Additionally, though the posterior pituitary gland doesn’t produce hormones on its own, it plays an important role in storing and secreting hormones that are produced by the hypothalamus, including oxytocin and antidiuretic hormone (ADH).
Specific hormones produced by the adrenal glands include:
Estrogens
Cortisol
Androstenedione
Testosterone
Pregnenolone
DHEA
Progesterone
Hormone function and change during menopause
We want to review a few key hormones that go through significant changes. We will talk about their functions, how their levels change during and after menopause, and what this means for the body’s function.
FSH - Follicle stimulating hormone (FSH) is made by your pituitary gland. It is important for sexual development and functioning. FSH is responsible for controlling the menstrual cycle and stimulates the growth of eggs in the ovaries. After menopause, this hormone tends to increase (3). FSH causes ovarian follicles to enlarge and produce estrogen. Over time, in menopause, these follicles become fewer, causing decreased levels of estrogen as women age. Because of this lack of estrogen production, FSH increases to produce more estrogen. Secondary to the lack of estrogen being made, there is no feedback to turn off the FSH production which makes it continuously elevated after menopause. Raised FSH and lower levels of estrogen may cause the characteristic hot flashes in menopause (4).
LH - Luteinizing Hormone (LH) is produced and released by the anterior pituitary gland and works to control the menstrual cycle. LH does this by aiding in ovulation (release of the egg from the ovaries). LH levels go up right before ovulation (5). Too little LH or too much LH can create problems with infertility and reproductive complications (6). During menopause, there is a reduction in estrogen which causes elevated LH levels (7).
The main takeaway here is that FSH and LH are on a negative feedback loop with estrogen. When women go through menopause, estrogen output decreases, therefore signaling an increase in FSH and LH.
Estrogens - The main source of estrogen comes from the ovaries, but adrenal glands and fat tissues can also make smaller amounts of estrogen. Estrogen is composed of estrone, estradiol, and estriol- the two latter estrogens are more important in hormone therapy. We will describe each briefly below. With decreases in estradiol and estriol, women may experience symptoms such as more frequent UTIs, vaginal pain, joint pain, headaches, memory loss, and mood changes to name a few.
Estrone -
Estrone comes from:
The ovaries
Fat tissues
Adrenal glands
Estrone is a weaker estrogen and tends to go up with the increased belly fat typical of menopause. Estrone can be inflammatory and an increase in levels is not ideal.
Estradiol - Estradiol plays a large role in puberty and reproduction and is the most powerful of the estrogens. It also plays an important role in bone health, cholesterol control, brain health, heart health, and skin health, as well as the health of other tissues in the body.
Estriol - Estriol is the weakest form of estrogen in the body. It typically increases during a pregnancy, though it is present throughout a woman’s lifetime. It decreases after menopause, and because it is a weaker form of estrogen, it can be helpful in hormone therapy, as it may alleviate some menopausal symptoms while also not increasing the risk of breast cancer (8).
Cortisol - With all of the changes that occur in the body, it’s not abnormal for cortisol levels to rise, as cortisol is commonly known as the “stress hormone.” However, if the adrenals focus on producing cortisol, they may not be able to produce the amount of hormone precursors needed for optimal function (9).
Androstenedione - Androstenedione is an important hormone in the production of testosterone and estrogen. The adrenal gland makes most of this hormone with only small amounts secreted by the ovary. After menopause, women produce nearly one half of the amount of this hormone as prior to menopause. This lowered production can have implications on the production of testosterone, which is needed for mood, skin, bone, and cognitive health (10).
Testosterone - As a normal process of aging, there is a reduction in testosterone in females. This decrease can be seen more specifically in women going through menopause. The ovaries play a significant role in the production of testosterone, but during menopause, there is a reduction in the hormones produced by the ovaries causing lower testosterone levels. Testosterone can also be produced in the adrenal glands (11). Lower levels of testosterone can affect women by impacting their energy levels, mood, sex drive, and cognitive function. Testosterone is very important for women as it helps with bone health, skin health, and nail health, and it has possible neuroprotective properties (12).
Pregnenolone - Pregnenolone is produced by the adrenal glands, produced by cholesterol in the body, and produced in the brain. It is considered a neurosteroid. It is also a precursor to progesterone as well as DHEA. DHEA then converts to androstenedione, which converts to testosterone and estrogen (13). Because its role as a hormone precursor is so important, it is often referred to as the “grandparent precursor” (14).
Pregnenolone has many important neurological functions, such as:
Neuroprotection (protection against nerve cell damage)
Neuroplasticity (the ability of neural networks in the brain to change through growth and reorganization)
Neurogenesis (growth and development of nervous tissue)
Regulating mood and memory (15)
Assisting with weight loss, libido, and overall energy
Like many other hormones, it decreases with age. Low levels of pregnenolone have been associated with depression, fatigue, low libido, loss of bone density, and loss of muscle mass. There is some promising research on the effects of pregnenolone therapy on conditions such as schizophrenia (16), depression (17), and memory loss (18).
Dehydroepiandrosterone (DHEA) - DHEA is an extremely important precursor hormone. It is synthesized from cholesterol through pregnenolone by the adrenal glands and can convert into other hormones, like testosterone and estrogen.
Levels of DHEA are typically highest when we are young adults and gradually decrease as we age, potentially as much as 80% less than our highest levels (19). Low levels of DHEA are associated with low libido, reduced bone mineral density, heart disease, and osteoporosis in women. On the other hand, sufficient levels of DHEA are associated with:
Brain health (20)
Immune function (21)
Energy
Bone metabolism (22)
Blood sugar regulation (23)
Healthy libido (24)
Progesterone - Progesterone plays a large role in menstrual cycles and signaling the uterus to thicken in the event of pregnancy. During and after menopause, progesterone levels decrease significantly. Progesterone is also able to counter the effects of cortisol in our bodies before menopause. After menopause, this cushion against cortisol weakens due to lack of progesterone. When you’re under high amounts of stress, your body also produces cortisol over progesterone, which can cause insomnia, low energy, digestion problems, weight gain, low sex drive, and more (25). Clinically, we have seen supplementation with progesterone help restore restful sleep in individuals with low progesterone, enhance energy, and increase sex drive (since it does convert into testosterone). Progesterone also helps to block aldosterone receptors which can promote water retention and swelling.
Recommendations for Hormone Replacement Therapy (HRT)
When the ovaries shut down, they no longer produce estrogen and progesterone. This means the adrenals have the heavy burden of taking over a lot of the hormonal work. Therefore, it’s important to support the adrenals before, during, and after menopause.
Importantly, if there is a thyroid issue that has not been addressed, the body will depend more on adrenals as well. If the body is already relying on the adrenals and then menopause occurs, women can run into a lot of issues. (This reinforces the need to check the thyroid and support it, if needed.) The thyroid gland has a strong influence over all the hormones (and more) that we have talked about.
As we discussed earlier, it may not be ideal to just directly take testosterone or estrogen, as there are some risks associated with taking ONLY these hormones, and you can also miss out on the benefits of the precursor hormones. At our office, we approach HRT with a holistic and functional medicine-based perspective. It is very important to us to look at the whole picture of the hormone cascade in order to provide the right hormonal support.
Hormones used in a functional medicine approach to HRT to support women during menopause may include:
Pregnenolone - As noted, pregnenolone is sometimes referred to as the “grandparent” precursor hormone. Once it’s synthesized, pregnenolone can be converted to DHEA or progesterone. DHEA can then be the precursor to androgens (testosterone and androstenedione) and estrogens through androstenedione. Progesterone can lead to the production of cortisol, aldosterone, androstenedione, estrogen and testosterone. Hence, the term “grandparent!” If you remember from earlier, pregnenolone is very important for neurological health, as well as the health of the liver, pancreas, pituitary gland, skin, and reproductive tissues (26). Pregnenolone is a wonderful hormone to take to support the endocrine system after menopause, under the guidance of a skilled practitioner.
DHEA - DHEA is synthesized from cholesterol through pregnenolone by the adrenals. It can counter potentially problematic hormones, such as cortisol, and it is a precursor to specific estrogens and testosterone. DHEA helps with brain health, memory, immune function, regulation of blood sugar, energy, and bone metabolism (26).
Progesterone - Progesterone is helpful to ease anxiety and provide calm. It is classified as a neurosteroid, and it helps the nervous system to function properly (27). It’s a great choice to take at night when women are having trouble sleeping and need help to resume a normal sleep cycle. It’s important to note that progesterone is the bioidentical form of progesterone, while progestin is the synthetic form and may not work the same as progesterone. In the research we noted previously that talked about the risks of HRT using estrogen, the participants were given estrogen combined with progestin instead of progesterone (28).
Estradiol - You might remember that estradiol is the strongest of the estrogens and can help with a myriad of issues. We use products that couple the estrogen with progesterone (not progestin). When estrogen is not balanced with progesterone, it can stimulate growth of the uterus lining. This can increase the risk of endometrial cancer (28).
Testosterone - We often see that DHEA feeds into testosterone, but there are times when it does not. In this case, we would make sure precursor hormones are adequate and refer out for testosterone replacement.
How do I know if I need HRT?
We recommend that women start getting hormone panels done yearly starting anywhere from 35-40 years old. This is often the time a hormonal decline can start and symptoms of this decline can creep in. Women should have a hormone panel run when they start to notice menopausal symptoms or are postmenopausal. Each hormone is influenced by another, so it’s important to run a full hormone panel.
How do you know if you are adequately dosed for HRT?
We will typically give a small starting dose and then build on that based on patient response and follow up hormone panels. Hormone panels can be done every 6-8 weeks, after the hormone has had time to build up in the blood and adequate blood levels are maintained. Maintenance hormone panels can be done every six months to a year to ensure that hormone levels continue to be appropriate.
What if I am taking hormones but have never been retested after starting?
Each time a new dose is given, it should be retested in 6-8 weeks to assess if the dose is enough or too much. We have often seen women come into the office who are on estrogen or another hormone who have blood levels far above lab range for HRT. This can be dangerous. As mentioned above, high estrogen can drive cancers. Proper clinical care for a patient includes retesting your recommendations for dosage to ensure levels are not too high or too low. We also think that this is where a lot of the concerns come from with HRT. Unfortunately, HRT has developed a bad reputation because of inadequate follow up testing. This misinformation has caused many women to miss out on HRT’s benefits.
We have seen the benefits of functional medicine-based HRT in our patients, and we are excited to support you in this journey to health. Please contact us if you have questions.
Works cited:
https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
https://medlineplus.gov/lab-tests/follicle-stimulating-hormone-fsh-levels-test/
https://medlineplus.gov/lab-tests/luteinizing-hormone-lh-levels-test/
https://ndnr.com/womens-health/the-relationship-between-adrenal-function-and-menopausal-symptoms-2/
https://www.healthline.com/health/low-testosterone-in-women#symptoms
https://www.yourhormones.com/proper-use-of-hormone-precursors/
https://www.healthspan.co.uk/advice/how-stress-affects-symptoms-of-menopause
https://www.yourhormones.com/proper-use-of-hormone-precursors/
https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372